About Us
HMS helps healthcare payers root out claims that are erroneous for any reason, at any stage in the claim cycle. Our payment integrity solutions address the full range of improper payments utilizing advanced analytics, leading technologies, and clinical expertise to deliver savings, compliance, and innovation. We enable plans and programs to avoid and recover improper payments, detect and prevent fraud, and ensure healthcare funds are used as intended for member care.
HMS is proud to be recognized for excellence in healthcare technology, data security, and service delivery. Our certifications and awards—including URAC accreditation, HITRUST certification, Best in KLAS recognition reflect our commitment to quality, compliance, and innovation in supporting recovery audit programs.
Recovery Audit Contractor (RAC) Program
The Medicaid Recovery Audit Contractor (RAC) program was established under the Affordable Care Act (ACA) in 2010. Its primary purpose is to reduce improper Medicaid payments by auditing provider claims to identify overpayments and underpayments. States are required to implement Medicaid RAC programs to ensure compliance with federal regulations and to improve the financial integrity of their Medicaid programs.
Medicaid RAC programs serve as a critical tool for states to recover funds lost to improperly billed claims, reinvesting these resources into Medicaid budgets to sustain and enhance the program’s effectiveness. By leveraging advanced analytics, clinical expertise, and robust data mining capabilities, Medicaid RAC vendors like HMS help states achieve these objectives while educating the provider community and minimizing provider abrasion.
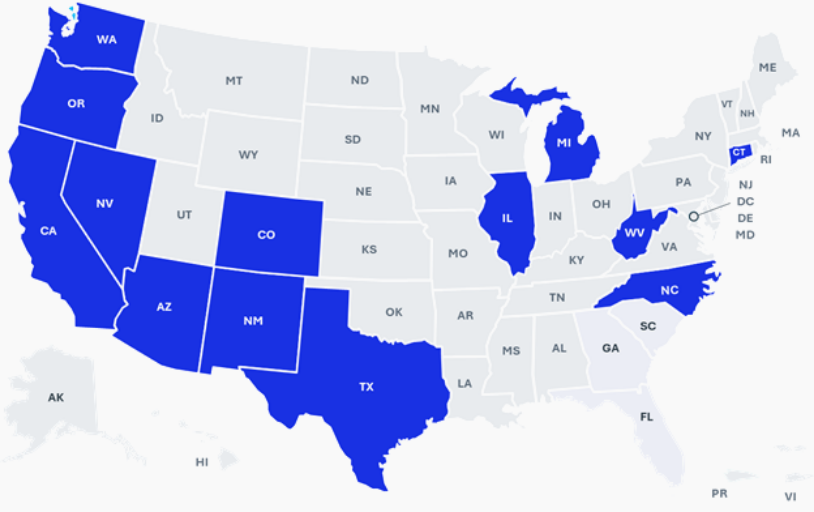
HMS Recovery Audit Contracts
$11.2 Billion
Total Recoveries & Savings
21+ Million
Cost Avoidance Records Delivered
210 Thousand
Clinical Reviews Completed
Our Payment Integrity solutions, also known as Program Integrity, address the full range of improper payments using advanced analytics, leading technologies, and expert clinicians. HMS deliver savings, compliance, and innovation for Medicaid, Medicare, commercial, and marketplace plans. We enable plans and programs to avoid and recover improper payments, detect and prevent fraud, and ensure healthcare funds are used as intended for member care.